Keloid
A keloid is an overgrowth of thick, rubbery skin that usually occurs at a site where the skin was previously injured. The keloid often grows much larger than the original injury and can be flesh-colored, redder, or otherwise darker. Though they are usually bothersome only for cosmetic reasons, they can sometimes be painful, itchy, or tingly. A dermatologist can remove the keloid, but this reinjures the skin and the keloid will often grow back. The injury to the skin that causes the keloid can be very minor. Some people develop a keloid after getting their ears pierced or even just scratching their skin.
Who's At Risk?
Keloids can appear in people of every race and ethnicity. Keloids can affect any person at any age.
Signs & Symptoms
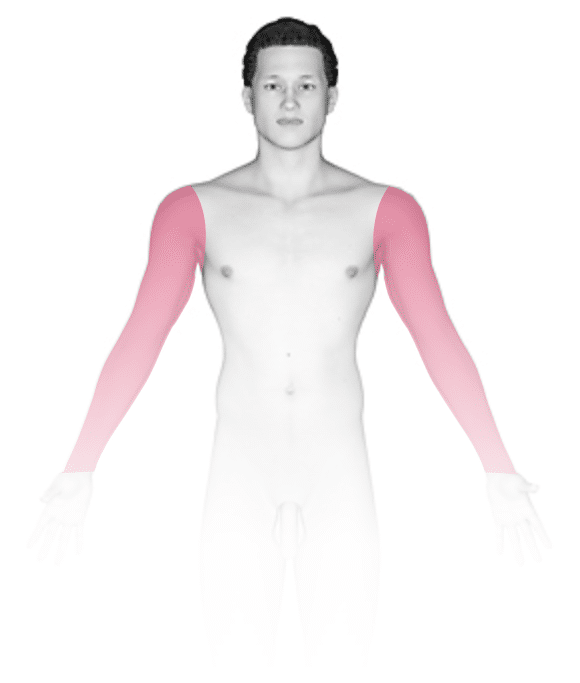
Keloids are usually seen on the neck, ear lobes, legs or arms, and on the upper trunk, especially the chest. They frequently follow the lines of injury. Spontaneous keloids are common on the mid-chest. Keloids are smooth and shiny, firm to the touch, red, hyperpigmented or skin-colored nodules with regular or irregular ridges. Keloids may develop projections that extend beyond the area of injury.
Self-Care Guidelines
None necessary except to avoid unnecessary skin injury, such as multiple piercing.
Treatments
Keloids are extremely difficult to treat, but your doctor may try the following:
- Some keloids respond to topically applied silicone sheeting.
- There has been some success in treating small earlobe keloids with pressure or “clip-on” earrings.
- Inflamed keloids often respond to steroid injections near the site. There is a risk of thinning of the skin (atrophy) with steroid injections.
Alternative therapies include:
- Freezing (cryosurgery) plus steroid injections.
- Surgery plus radiation therapy to the affected area. Surgical removal (excision) of keloids may lead to the keloid coming back (recurring) larger than it was before the excision.
- Laser therapy with a pulsed-dye laser to actively expanding lesions.
- Other injectable agents, such as interferon alpha and gamma.
Visit Urgency
Seek medical evaluation if keloids become bothersome or symptomatic.
References
Bolognia, Jean L., ed. Dermatology, pp.1531-1535. New York: Mosby, 2003.
Freedberg, Irwin M., ed. Fitzpatrick’s Dermatology in General Medicine. 6th ed, pp.991-992, 2475. New York: McGraw-Hill, 2003.
Last modified on August 16th, 2022 at 2:45 pm
Not sure what to look for?
Try our new Rash and Skin Condition Finder





